Up to 58 million Americans have actinic keratosis (AK). An AK has the potential to progress to squamous cell carcinoma (SCC), the second most common skin cancer. While most AKs remain benign, approximately 10 percent develop into SCC within an average of two years.1 Since there is no way to know ahead of time which ones will become cancerous, it is very important to seek a dermatologist’s care. Frequent skin examinations are the key to early detection and prevention.
What are Actinic Keratoses (AKs)?
AKs – often called “sun spots”— are rough-textured, dry, scaly patches on the skin caused by excessive exposure to ultraviolet light (UV) such as sunlight. They occur most often on sun exposed areas such as the face, scalp or ears, and can range in color from skin toned to reddish brown. They can be as small as a pinhead or larger than a quarter.
What do AKs look like?
Actinic Keratoses generally begin as rough spots of skin that may be easier felt than seen. Common complaints include a lesion that has increased in size or one that is raised, bleeding, poor in healing, discolored, or associated with discomfort such as pain or itching.
While a lesion may initially appear skin colored to pink, red, or brown, lesions on darker skin may be more pigmented. AKs may feel soft, rough, or “gritty,” but in any case, they feel different from the surrounding healthy skin.
Since there are many clinical variants of AKs, it is best to consult a dermatologist if you suspect a lesion.

Who gets AKs?
AKs are seen primarily in Caucasians with pale skin living in sunny climates. Areas of the skin with the most sun exposure, such as the head, neck, forearms, and hands account for more than 80 percent of AKs.
Actinic Keratoses develop as the result of years of sun exposure. Because the effect of sun exposure is cumulative, it is your lifetime exposure that increases your risk. Even if you didn’t suntan much, years of just doing simple tasks outside can add up to significant amount of sun exposures.
For example
- Going out to the mailbox
- Playing an outdoor sport
- Walking the dog
Because AKs take a long time to develop, they generally appear after the age of 40. The American Academy of Dermatology estimates that 60 percent of persons apt to get Actinic Keratoses will indeed get at least one AK in their lifetime.
Your risk of developing AKs increases if you have one or more of the risk factors.
What are some of the risk factors?
- A history of cumulative sun exposure
- Fair skin
- Blond or red hair, in particular if combined with blue, hazel or green eyes
- A tendency to freckle or burn after sun exposure
- A weakened immune system
Important Risk Information
What is LEVULAN KERASTICK used for?
The LEVULAN KERASTICK for Topical Solution plus blue light illumination using the BLU-U Blue Light Photodynamic Therapy Illuminator is indicated for the treatment of minimally to moderately thick actinic keratoses of the face or scalp.
Who should NOT take LEVULAN KERASTICK?
LEVULAN KERASTICK should not be taken by patients who have cutaneous photosensitivity at wavelengths at 400-450 nm, porphyria, or known allergies to porphyrins, and in patients with known sensitivity to any of the components of the LEVULAN KERASTICK for Topical Solution.
LEVULAN KERASTICK has not been tested on patients with inherited or acquired coagulation defects. There have been no formal studies of the interaction of LEVULAN KERASTICK for Topical Solution with any other drugs and no drug-specific interactions were noted during any of the controlled clinical trials. It is possible that concomitant use of other known photosensitizing agents might increase the photosensitivity reaction of actinic keratoses treated with the LEVULAN KERASTICK. It is important to tell your physician if you are taking any oral medications or using any topical prescription or non-prescription products on your face or scalp. Tell your doctor if you are pregnant or nursing.
What are the possible side effects?
The most common side effects include scaling/crusting, hypo/hyper-pigmentation, itching, stinging, and/or burning, erythema and edema. Severe stinging and/or burning at one or more lesions being treated was reported by at least 50% of patients at some time during the treatment.
What precautions should be taken?
Patients should avoid exposure of the photosensitive treatment sites to sunlight or bright indoor light for at least 40 hours after application of LEVULAN KERASTICK. Exposure may result in a stinging and/or burning sensation and may cause erythema or edema of the lesions. Sunscreens will not protect against photosensitivity reactions caused by visible light.
LEVULAN KERASTICK and BLU-U® Photodynamic Therapy (PDT):
A Unique Therapeutic Approach to Manage Actinic Keratoses
What is LEVULAN KERASTICK and BLU-U PDT?
LEVULAN KERASTICK and BLU-U PDT is an in-office therapy that provides high clearance with low downtime for appropriate actinic keratosis patients.*1
Who are appropriate AK patients?
- Patients with few minimally to moderately thick AKs of the face or scalp
- Patients with multiple minimally to moderately thick AKs of the face or scalp
- Patients with minimally to moderately thick AKs in sensitive areas on the face or scalp
Why is patient adherence important?
Appropriate patient selection requires the evaluation of a range of factors, such as AK lesion characteristics, patient expectations, patient history and patient adherence. Patient adherence is closely linked to treatment outcome which makes patient selection very important in order to reduce risk of nonadherence.
Among the patients at risk for nonadherence are those who:
- Are elderly
- Have asymptomatic disease
- Have poor understanding of the condition
- Lack belief in benefit of the treatment
Among the factors associated with nonadherence are:
- Side effects or fear of side effects
- Complexity of the drug regimen
- Cost of treatment/poor health coverage
Poor medication adherence is reaching crisis proportions in the US
A 2009 survey by the Senior Citizens League found
- 42% of the elderly had either postponed filling their prescription or were reducing their dosage
Another survey found
- 3 of every 4 American consumers report not always taking their prescription medicine as directed
- 49% said they had forgotten to take a prescribed medicine
- 31% had not filled a prescription they were given
- 24% had taken less than the recommended dose
Why choose LEVULAN KERASTICK and BLU-U PDT?
PDT is an effective therapy that will not only add value for your practice, but it may also be the right treatment choice for your new AK patients or those who are unwilling to repeat a prior topical treatment. In addition, an in-office therapy can impact patient adherence.
- PDT is initiated and completed in an in-office setting
- Physician-controlled treatment is administered by a qualified healthcare professional**
- No prescription for the patient to fill
- No daily medication for the patient to remember
- The 2-part, 2-office visit treatment is completed in less than 24 hours
- Recovery begins when treatment ends
BLU-U® Clinical Indications
- The BLU-U Blue Light Photodynamic Therapy Illuminator is generally indicated to treat dermatological conditions.
- In combination with the Levulan® Kerastick® (aminolevulinic acid HCl) for Topical Solution, 20%, the BLU-U is indicated for the treatment of minimally to moderately thick actinic keratoses of the face or scalp.
- The BLU-U is also specifically indicated to treat moderate inflammatory acne vulgaris. When using the BLU-U for acne, do not use this device with photosensitizing drugs.
BLU-U® – Unique and Patented Design

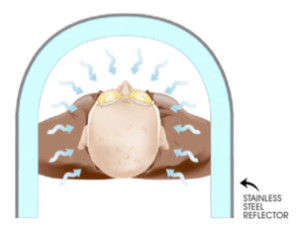
The BLU-U for actinic keratoses (AKs) – optimal design for treating AKs on the face or scalp
Clinical Output
- As you know, AKs reside within the epidermis which is less than 2 mm thick.1 The BLU-U blue light penetrates up to 2 mm of skin.2
- The BLU-U also has enough energy to produce a photodynamic response. In our Phase II study the maximum clinical response with Levulan® Kerastick® (aminolevulinic acid HCl) Topical Solution, 20% was produced at 10 J/cm2 at 1000 seconds.
- Finally, BLU-U output is matched to the highest absorption peak of PpIX.3 It’s peak wavelength occurs at 417 ±5 nm and the maximum absorption peak for porphyrins occurs at 410 nm.3,4
Design Features
The BLU-U is designed to deliver a uniform light dose and stable wavelength to an entire treatment area.3
- The large U-shaped design and tube spacing allows for the treatment of an entire face or scalp while delivering a consistent light dose all the way to the treatment edges.
- The unit is designed with a stainless steel reflective wall behind the tubes to minimize loss of light within the U-shaped treatment area.
- Light tubes are spaced much closer together at the top and bottom than in the middle to compensate for light falloff in this area.
The BLU-U is designed to deliver a consistent light dose.3
- The phosphor in the fluorescent tubes produces a very stable and cost-effective wavelength.
- The BLU-U contains a microprocessor that continuously monitors and adjusts light output to maintain dose stability from the first to the last treatment.
Use with eyewear that blocks light of at least 500 nm and shorter with an optical density of two or greater.
BLU-U does not emit UVA or UVB light.
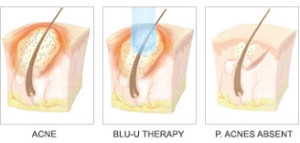
BLU-U for Acne – Innovative, Simple, Effective
The BLU-U offers effective, non-invasive and pain-free blue light treatment for moderate inflammatory acne vulgaris. Narrow band blue light causes a photodynamic effect within the pilosebaceous gland that kills P. acnes, the bacteria primarily responsible for acne vulgaris. When used in a series of brief (approximately 17 minutes) exposure sessions, it provides a simple, non-invasive treatment regimen. BLU-U treatments can be a primary treatment, an alternative to pharmaceuticals and topicals, or an adjunct to skin care programs.
FAQs: BLU-U® Blue Light Photodynamic Therapy Illuminator
What is Photodynamic Therapy (PDT)?
PDT is the use of light-activated drugs which produce singlet oxygen to treat diseased tissues. The drug undergoes a chemical reaction when light of a particular wavelength and intensity is applied, resulting in a therapeutic effect.
Is the BLU-U a laser?
No, the BLU-U is not a laser. Lasers deliver light as coherent beams, while the BLU-U delivers incoherent light scattered over a larger area.
Who performs the BLU-U light therapy procedure?
A qualified healthcare provider is required to perform the procedure.
How much space is required for the BLU-U?
In its open position the BLU-U footprint is approximately 3’ x 3’. We recommend a treatment area of 7’ x 9’ for convenience. When stored, the BLU-U only requires a 2’ x 3’ storage space. See Unit Specifications.
Will I receive reimbursement for BLU-U services?
Reimbursement for BLU-U therapy for actinic keratoses is available. For reimbursement support you may contact any one of our DUSAdelivers team members.
Does the BLU-U come with a warranty?
Yes, a BLU-U has a 3-year warranty on all parts and labor. Please contact our Customer Servicedepartment for additional information.
What indicates the BLU-U is ready to be used?
The system is ready for use when the Keyswitch is turned to the “l” (on) position and the System Status Indicator flashes three times and goes off. See the BLU-U Operating Manual for more specific details.
Is it recommended that the patient have appropriate eye protection?
Yes. Although exposure to the light from the BLU-U during a patient treatment is below the recommended maximum skin and eye exposure for blue and UV light, it is recommended that both the patient and clinician(s) wear blue-blocking eye protection while the BLU-U is in operation for comfort and to further minimize eye exposure.
Does the patient need to be watched for the entire session?
We recommend that the patient and the BLU-U indicator light be monitored throughout the treatment.
What expectations should be set for the patient prior to BLU-U light therapy?
See Patient Education for properly setting patient expectations.
Is it possible to stop the therapy midway through a session?
Yes, if a patient needs to remove himself from the unit, or asks for it to be turned off, he can do so at any time. Once the light treatment is stopped, it is not to be resumed during the session.
